HPV Vaccine: Age, Schedule, Importance & Side Effects - Cleveland Clinic
The HPV vaccine is a series of shots that can protect you from an HPV (human papillomavirus) infection. HPV is a common sexually transmitted infection (STI) that spreads through skin-to-skin contact. There are about 40 types (strains) of HPV that can spread through sex. It's so common that 80% of sexually active people will have an HPV infection at some point. Often, healthy immune systems can fight off the virus.
But some HPV infections don't go away. Some progress to cancer. For example, most cervical cancer and cancers affecting your genitals are associated with an HPV infection. HPV infections are also responsible for genital warts.
This is why getting the HPV vaccine is so important. It's a safe and effective way to prevent infections if you're ever exposed.
What is the HPV vaccine for?
The HPV vaccine prevents HPV infections that can progress to cancer or genital warts. This part's important: The vaccine prevents infections, but it isn't a treatment. If you've already been exposed to a particular strain of HPV, the vaccine can't heal the infection.
The HPV vaccine can protect you from strains you haven't encountered before. These include high-risk types and low-risk types. High-risk HPV strains can progress to cancer. Low-risk types don't increase your cancer risk, but they can cause nuisance conditions like genital warts.
The HPV vaccine prevents infections that can lead to:
But, not all HPV vaccines provide the same protection. There are three different vaccines. Each protects against different strains of HPV.
Two of the vaccines are no longer available in the U.S. but are available in other countries. Still, many people in the U.S. received these earlier vaccines. It's important to understand what protection you have based on the vaccine you received.
Gardasil-9
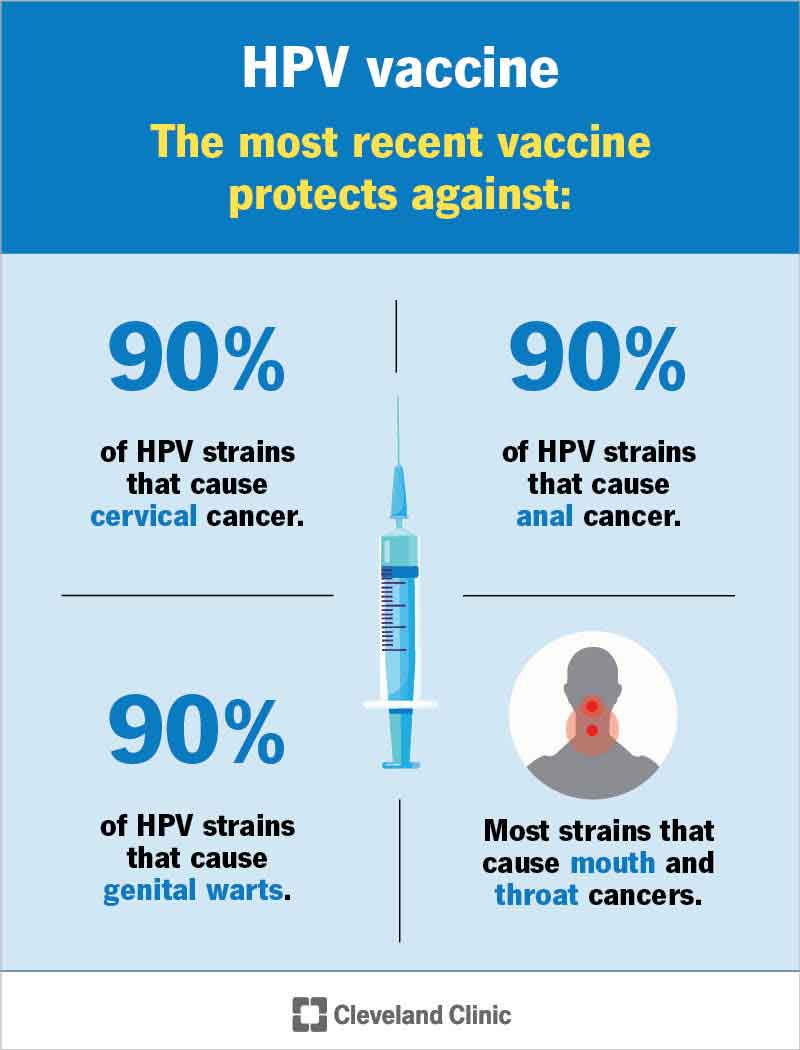
Since 2017, Gardasil-9 has been the only HPV vaccine available in the United States. It provides the most comprehensive protection of any HPV vaccine. Gardasil-9 protects against infections associated with:
- HPV-16 & HPV-18. These are the two most common high-risk strains of HPV. These strains cause 70% of cervical cancers, 90% of anal cancers and many cancers that can affect your throat and genitals.
- HPV-31, 33, 45, 52 & 58. Together, these strains cause an additional 20% of cervical cancers.
- HPV-6 & HPV-11. These strains cause 90% of genital warts. They're considered low risk since they don't cause cancer. Still, genital warts are a nuisance — and contagious. The vaccine can prevent you from ever having to deal with them yourself or having to tell a partner that you exposed them.
Gardasil
Gardasil was the first FDA-approved HPV vaccine. It became available in 2006. Gardasil protects against infections associated with:
- HPV-16 & HPV-18 (associated with 70% of cervical cancers, 90% of anal cancers and many cancers that can affect your throat and genitals).
- HPV-6 & HPV-11 (associated with 90% of genital warts).
Unlike Gardasil-9, the original Gardasil doesn't protect against the additional HPV strains that cause 20% of cervical cancers. So, while Gardasil-9 reduces your risk of cervical cancer by 90%, the original Gardasil reduces your risk by 70%.
Cervarix
The FDA approved Cervarix in 2009. Cervarix only protects against high-risk strains of HPV associated with cancer. It doesn't protect you from the strains that cause genital warts. Cervarix protects against infections associated with:
- HPV-16.
- HPV-18.
Who should get the HPV vaccine?
Everyone, regardless of sex or gender, should get vaccinated before they're exposed to HPV through sexual activity. Remember — the HPV vaccine can only protect you from strains of HPV you haven't already been exposed to via an infected partner.
The age recommendations from the Centers for Disease Control (CDC) for getting the vaccine reflect this rationale.
- Children between ages 11 & 12. The HPV vaccine is part of the vaccination schedule for children between 11 and 12, but children as young as 9 years old can safely receive it. The goal is to vaccinate children before they become sexually active and risk exposure.
- Adults up to and including age 26. The vaccine is also recommended for adults up to age 26. This includes people who started the series as a child, teen or young adult but didn't finish it.
- Some adults up to and including age 45: In 2018, the Federal Drug Administration (FDA) expanded the age range from 26 to 45. The recommendation was based on research that showed the vaccine prevented HPV infections among adults in this age range, too.
The age limit for getting vaccinated (first 26 and now 45) is based on the thinking that most people have had sex (and potentially been exposed to multiple strains of HPV) by adulthood. If you've already been exposed, the vaccine won't provide much benefit. Related, not all insurance companies cover the costs of the vaccine past ages 26 or 45.
But this doesn't mean you can't personally benefit from the vaccine if you're a middle-aged adult. For example, if you've had few or no previous partners, getting vaccinated can potentially protect you from HPV if you're about to start a sexual relationship.
Everyone's situation is different. Your healthcare provider can advise you based on your sexual history.
Who shouldn't get the HPV vaccine?
You shouldn't get the HPV vaccine if you:
- Are pregnant. There isn't a lot of research about the vaccine's safety during pregnancy, so it's best to get it after having your baby. But if you learn you're pregnant after getting a shot, don't worry. The HPV vaccine isn't associated with pregnancy complications.
- Had a reaction to a previous dose. Tell your healthcare provider if you had a reaction to a previous HPV shot or to the ingredients in it. Inform them of any severe allergies you have, including yeast or latex allergies, which may increase your risk of an allergic reaction.
- Have moderate to severe illness. You may need to wait to get the vaccine until you're healthy. Ask your provider when it's safe to get the shot.
Comments
Post a Comment