What do genital warts look like? Symptoms and treatments - Medical News Today
What do genital warts look like? Symptoms and treatments - Medical News Today |
| What do genital warts look like? Symptoms and treatments - Medical News Today Posted: 02 Feb 2021 09:26 AM PST  Genital warts are flesh colored bumps that can appear on or around the genitals. The sexually transmitted infection (STI) human papillomavirus (HPV) is what causes them. Once a person has genital warts, HPV can transmit to others, even if the person has no symptoms. This article will cover what genital warts look like, as well as some causes and treatment options. It will also discuss outlook, some similar conditions, and when to contact a doctor. Genital warts can appear on or around the genitals. Possible locations include the following:
These warts can also appear in the mouth or throat if someone has had oral sex with a person who has them. Genital warts look similar to the warts that a person might get on their hands or elsewhere on the body. This is because various strains of HPV cause all warts, including genital warts. Genital warts can appear weeks, months, or even years after an HPV infection. Some people with HPV have no symptoms at all. For this reason, the fact that a person has not had recent sexual contact does not exclude the possibility of having genital warts. Genital warts do not cause sores, bleeding, or open wounds unless a person scratches them or they catch on something. Discolored marks, rashes, or bleeding on or around the genitals usually indicate the presence of something else, such as herpes or a skin infection. Some symptoms that suggest that the bumps on the genitals might be genital warts include the following:
HPV causes genital warts. This is the most common STI in the United States. The strain of HPV that causes genital warts spreads through skin-to-skin contact with someone who has it, often during vaginal, anal, or oral sex. However, genital warts can still spread without penetration and if a person does not have symptoms. Any anal, vaginal, or penile contact may spread HPV. This can happen even if a person has no HPV symptoms. Condoms do not fully protect against HPV, since they do not cover all of the areas of the body that may spread the infection. They can, however, reduce the chance of HPV spreading. Genital warts are not dangerous, though a person might not like how they look. A different strain of HPV from the one that causes genital warts may increase the risk of cancer. That strain of HPV correlates with a higher risk of certain cancers, including: According to the World Health Organization (WHO), "nearly all cases of cervical cancer can be attributable to HPV infection." The strain of HPV that causes genital warts is a low risk strain for cervical cancer, but other HPV strains are higher risk. People who have genital warts may also have a strain of HPV that increases their risk of cancer. Some people with genital warts say that they feel similar to tiny, bumpy cauliflowers. The outer surface of the warts may feel smooth or rough. The warts may grow or change texture a little before they clear up. These warts do not usually hurt, but the skin under the wart may feel itchy. If the warts catch on something, such as underwear, they may hurt. Genital warts will not bleed if a person does not disturb them. However, friction from walking or sex can irritate or tear the warts. Warts may open, bleed, or become infected from friction or if they snag on something. The presence of bumps on or around the genitals does not necessarily mean that a person has HPV. Some other potential causes of genital bumps include: No test can reliably detect HPV for both sexes. However, in females, doctors can test for HPV during cervical cancer screenings with a Pap smear. For many people, doctors will diagnose the condition based on symptoms, after ruling out other potential conditions. A person should contact a doctor if they:
Certain tests can look for cancer related to HPV. A doctor may recommend undergoing regular Pap smears or other tests based on a person's history of genital warts. Because it is impossible to self-diagnose HPV, it is important to contact a doctor about any unusual or new growths on the genitals, even if the person thinks that they have had no HPV exposure. It is possible to vaccinate both females and males against some types of HPV, including those that cause most cervical cancers. Experts usually recommend that people receive the vaccine before they become sexually active and have exposure to any strains of HPV. However, some younger adults may still benefit from vaccination. Anyone who is interested in having themselves or their child vaccinated should consult a doctor. HPV is a chronic virus with no cure. This means that a person may periodically develop genital warts for the rest of their life. Not all people with HPV develop genital warts, however, and even those with a history of wart outbreaks may never again have another outbreak. There are treatments available for genital warts. For example, a doctor may recommend prescription creams to clear up the infection. If the warts become infected or cause a skin infection, they may also recommend an antibiotic. The cancers that HPV increases the risk of are also treatable. So, a person should contact a doctor early about any symptoms of cancer or unusual growths. Females with HPV may need more frequent cervical cancer screenings. HPV is a common infection, and many people who contract the virus never know that they have it. People with genital warts should assume that they are contagious and discuss risk and risk mitigation strategies with their partners. A doctor can help with assessing risk and recommending treatment options. |
| 4 Important Things Everyone Should Know About HPV (Human Papillomavirus) - TheBody.com Posted: 06 Jan 2021 12:00 AM PST 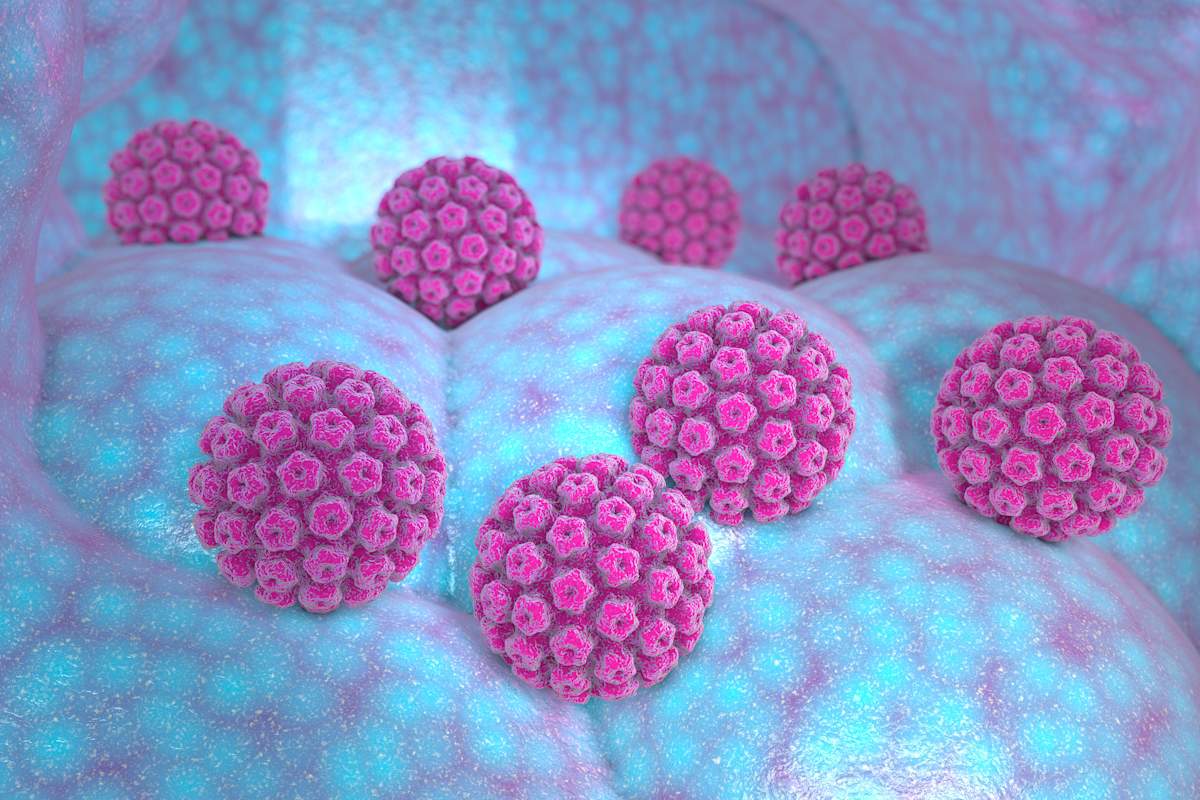 Here is the piping hot tea: 80% to 90% of sexually active people will have some strain of HPV (human papillomavirus) at some point in their lives. Not only is HPV the most common sexually transmitted infection (STI), it's one of the most common viruses that exist on this, the planet Earth. If the term "STI" scares you, it really shouldn't. Yes, HPV is an STI, but the vast majority of cases of HPV go away all on their own about 90% of the time. "I always tell my patients that HPV is a natural consequence of being sexually active. Although there are some measures you can take to reduce risk of transmitting or acquiring HPV, most sexually active people will be exposed at some point," says sexual health expert Ina Park, M.D., author of Strange Bedfellows, a book on STIs. While very common and, in most cases, quite innocuous, some high-risk HPV strains can lead to certain cancers and/or genital warts. HPV does not appear on a regular STI panel, is spread via skin-to-skin contact, and has no cure. The only things we can currently do to curb the spread of HPV is to vaccinate children; use barrier methods, such as condoms; and have regular Pap smears—for those of us who own a cervix. People are generally pretty confused about HPV and how it works. As a certified sex educator, I find myself regularly holding the hands of friends, family, clients, and readers alike when they come face-to-face with HPV. I'm asked the same questions over and over again. Why? Because it's an STI, which means there is stigma surrounding this very common virus. People are afraid to talk about HPV, when it is as ordinary as getting a cold. When we don't talk about it, we can only do harm. Information is power. Here are some important, albeit rarely talked about, things everyone should know about the human papillomavirus. The HPV Vaccine Doesn't Prevent All Forms of HPVGardasil, the HPV vaccine, is highly effective in preventing nine high-risk strains of the human papillomavirus. Health care professionals recommend that young people, regardless of gender, should get the HPV vaccine around the ages of 11 to 13 as a preventative measure. You can get the vaccine up until the age of 26. Some 27 to 45 year olds who are not already vaccinated may get the HPV vaccine after talking with their doctor. While the Vaccine is Critically Important to Public Health, It Is Not a Get-Out-of-HPV-Free CardThere are over 100 known strains of HPV, with new ones showing up and mutating all the time. This is common behavior for a virus: They adapt and change over time. Of the strains we currently know about, Felice Gersh, M.D., director of the Integrative Medical Group of Irvine and the author of PCOS SOS Fertility Fast Track, tells TheBody that 40 strains are considered "high risk." This means that you can have the Gardasil vaccine, contract an HPV strain that isn't among the nine strains the vaccine protects against, and therefore still be at risk for cervical and/or other cancers. Ninety percent of cervical cancer is related to cell changes caused by an HPV infection. If you have regular Pap screenings, cell changes can be detected early enough to have treatment. If everyone had regular Pap smears and screenings, cervical cancer could be completely eradicated. What a wonderful world that would be. HPV Is Not a Cis-Female-Only VirusWhat's more, Gersh tells us HPV doesn't only affect cervical health. It is also responsible for cancers of the vulva, vagina, anus, oral cavity, and throat. While regular Pap screenings are the only way we currently screen for HPV, that does not mean it only affects the cisgender female population. The Centers for Disease Control and Prevention (CDC) says that in addition to HPV-related cervical cancer, the virus is also thought to be responsible for 90% of all anal cancers and 70% of oropharyngeal and vulvar/vaginal cancers. "In fact, HPV-related oropharyngeal cancer (back of the throat/tonsils/base of the tongue) is now more common in the U.S. than cervical cancer," says Park. "Those cancers are almost five times more common in men than women." TLDR; HPV affects every single sexually active human, regardless of one's genitals. Intercourse Is Not the Only Way to Get HPVWhile having sexual intercourse is the most common way this virus is spread, it is by no means the only way. Unlike STIs like HIV, chlamydia, or gonorrhea, HPV is spread "through direct contact, not through bodily fluids. Typically, the contact is genital skin to genital skin, penile-vaginal penetration, anal penetration, and oral sex (mouth to genitals)," Gersh explains. Anne Hodder-Shipp, ACS, a certified sex educator and founder of Everyone Deserves Sex Ed, tells TheBody that HPV "can be spread through skin-to-skin contact, really any mucus membrane coming in contact with the virus." The genitals are a prime region for HPV because the soft, absorbent tissue of the genital region is among the most absorbent on the human body. According to research published in The Lancet, a leading medical journal, while it's pretty rare to spread HPV from hand-to-genital contact, it is possible. This means you could, in fact, touch someone's genitals and then your own, contracting HPV from the hand carrying the virus. This is not meant to be a scare tactic designed to frighten you into celibacy. It is merely a realistic look at the virulent nature of HPV. It is really effing contagious! Your Immune System Plays a Big Role in Your Ability to Fight off HPVThe way your body responds to HPV infection is correlated with the strength or weakness of your immune system. While some strains of HPV are far more aggressive than others, their viral makeup is not the only thing that dictates how it will impact your body. There is no cure for HPV. In the vast majority of cases, your body will fight off the virus by itself. This means your immune system is a key player in your ability to eradicate this virus. This is troubling for people who are immunocompromised, such as some people living with HIV, lupus, or other immune-related illnesses. "The status of one's immune system has a definite impact on the outcome of an infection," Gersh explains. "A healthy and robust immune system is most likely to successfully resolve an HPV infection. When the immune system is not robust and healthy, the propensity for an infectious virus to create a precancerous state of the tissues increases, and in the case of HPV, low-grade HPV lesions (warts) would also become more likely." This is certainly not to say that people with weaker immune systems shouldn't have sex—that would be bonkers—but if you do have a compromised immune system, you may want to discuss your HPV risk with your medical provider and schedule more regular Pap screenings, if you own a cervix. At the end of the day, we're all going to get HPV if we have sex. The best defense we have against this virus is information. So, let's stop being so afraid to talk about it. |
| You are subscribed to email updates from "hpv in men" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment