Human Papillomavirus (HPV) may be a cause of Cancer in both men and women - Northeast Now
Human Papillomavirus (HPV) may be a cause of Cancer in both men and women - Northeast Now |
- Human Papillomavirus (HPV) may be a cause of Cancer in both men and women - Northeast Now
- HPV Prevalence Higher in Adults With More Than 5 Lifetime Sexual Partners - infectiousdiseaseadvisor.com
- Ask the Doctors: Boys, girls can benefit from HPV vaccine - Santa Maria Times
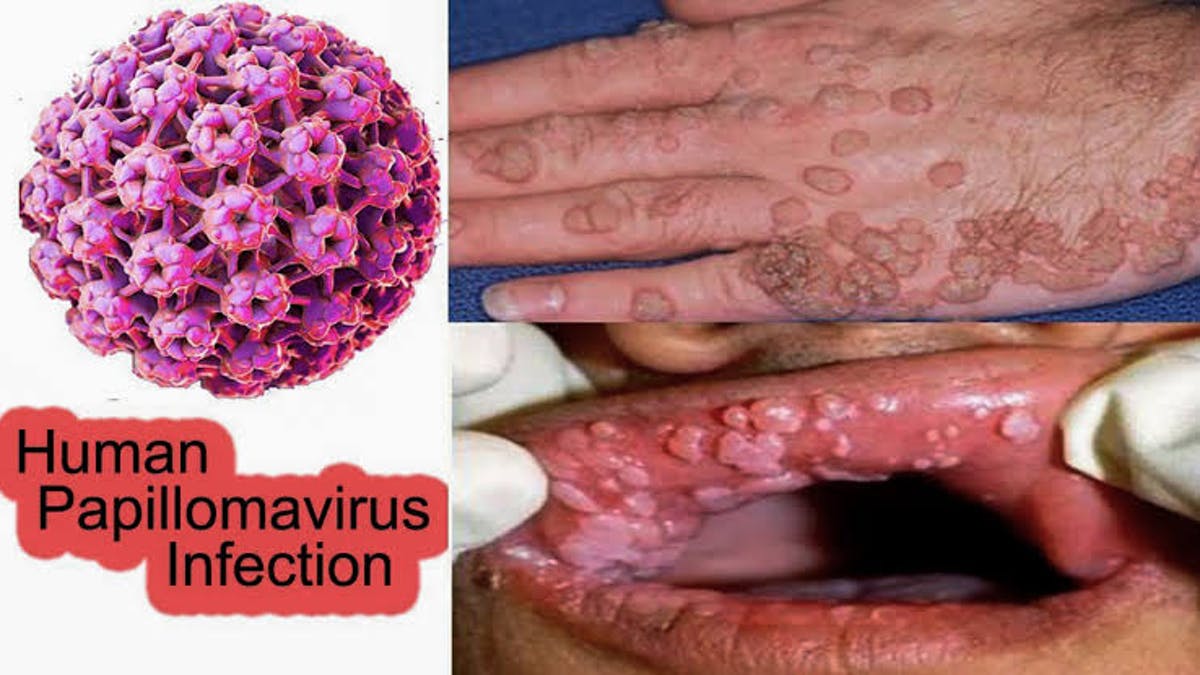
| Human Papillomavirus (HPV) may be a cause of Cancer in both men and women - Northeast Now Posted: 25 Aug 2020 12:35 AM PDT Scientists worldwide have started talking about the Human Papillomavirus as it may cause cancer. Human papillomavirus (HPV) is a viral infection transmitted between people through skin-to-skin contact. There are over 100 varieties of Human papillomavirus, and more than 40 of which are passed through sexual contact. It affects the genitals, mouth, or throat. Some types of Human papillomavirus can lead to the development of genital warts and even cancers of the cervix, anus, and throat. The virus that causes Human papillomavirus infection is transmitted through skin-to-skin contact. Most people get a genital HPV infection through direct sexual contact, including vaginal, anal, and oral sex. Many people have Human papillomavirus and don't even know about it. It may contract it even if your partner doesn't have any symptoms. In rare cases, a mother who has Human papillomavirus can transmit the virus to her baby during delivery. The child may develop a condition called recurrent respiratory papillomatosis where they develop warts inside their throat or airways. Human papillomavirus symptoms
Often, Human papillomavirus infection does not show any noticeable symptoms, and the infections go away on their own within two years. When the virus doesn't go away on its own, it can cause serious health problems. These include genital warts and warts in the throat (known as recurrent respiratory papillomatosis). Human papillomavirus can also cause cervical cancer and other cancers of the genitals, head, neck, and throat. The types of Human papillomavirus that cause warts are different from the types that cause cancer. Cancers caused by HPV often don't show symptoms until the cancer is in later stages of growth. Also Read – COVID19: No change to closure of Meghalaya’s entry points in first week of every month Many men that are infected with HPV have no symptoms, although some may develop genital warts. See your doctor if you notice any unusual bumps or lesions on your penis, scrotum, or anus. More than 80 percent women will contract at least one type of HPV during their lifetime. Genital warts appear inside the vagina, in or around the anus, and on the cervix or vulva. |
| Posted: 12 Aug 2020 12:00 AM PDT  Among sexually experienced adults, prevalence of human papillomavirus (HPV) infection was primarily reflective of higher number of lifetime sexual partners, specifically >5 lifetime sexual partners, according to study results published in Clinical Infectious Diseases. Using data from the 2013-2016 National Health and Nutrition Examination Survey (NHANES), researchers examined the relationship between current and past sexual behaviors on prevalent burden of HPV infection stratified by sex, age group, and number of lifetime sexual partners. The analysis included 5093 participants aged 18-59 years who had an evaluable HPV test, reported at least 1 lifetime sexual partner, and had not received an HPV vaccination. The primary outcomes included the crude prevalence of genital vaccine-type HPV, defined as the detection of ≥1 genotype in the Gardasil-9 vaccine (6, 11, 16, 18, 31, 33, 45, 52, or 58), genital high-risk HPV infection defined as the detection of ≥1 high-risk HPV genotype (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, or 68), and any genital HPV infection defined as the detection ≥1 of the 37 possible genotypes. Since the HPV vaccine is presumed to prevent only newly acquired infections, the crude prevalence of each outcome was also calculated after excluding participants at highest risk for newly acquired infection, defined as those who reported a new sexual partner within the past 12 months. Among both men (n=2495) and women (n=2598), the distribution of race/ethnicity, marital status, and cigarette smoking status varied substantially by age group. Among men, the median number of lifetime sexual partners increased with age: 5 for persons aged 18 to 26 years, 8 for persons aged 27 to 45 years, and 10 for persons aged 45 to 59 years (interquartile range [IQR] 3-12, 3-19, and 5-20, respectively). Among women, the median number of lifetime sexual partners was 5 across all age groups. Conversely, the proportion reporting a new sexual partner in the past 12 months substantially decreased with older age in both men and women: 40.7% and 28.4% among persons aged 18 to 26 years, 16.6% and 10.5% among persons aged 27 to 45 years, and 9.3% and 3.5% among persons aged 45 to 59 years, respectively. Continue Reading In each age group, genital HPV prevalence was higher among persons with >5 lifetime sexual partners compared with 1 to 5 lifetime sexual partners in both men and women. There were only slight reductions in HPV prevalence after removing participants who reported a new sexual partner in the past 12 months. Among men with >5 lifetime sexual partners, the adjusted prevalence of 9-valent vaccine type HPV infection was 20% in the full group (95% CI, 16.6-23.3) compared with 18.8% (95% CI, 15.0-22.6) among those with no new sexual partners. Among women with >5 lifetime sexual partners, the adjusted prevalence of 9-valent vaccine-type HPV infection was 13.4% in the full group (95% CI, 9.9-17.0) compared with 12.1% (95% CI, 8.8-15.4) among those with no new sexual partners. Despite having a large nationally representative sample, there were some notable limitations. Not all individuals provided genital samples or questionnaire data. While NHANES is the largest population-based survey of HPV prevalence, the sample size was still insufficient to allow for more granular stratification of lifetime sexual partners and age. Plus, since DNA extraction method used in NHANES results in an increased test sensitivity, this "may explain why HPV prevalence is relatively high in older adults, such as post-menopausal women, who may be more likely to have low viral load infections," noted the researchers. "Thus, when discussing the risks/benefits to vaccination of adult men and women for clinical decision making, it will be important to incorporate the likely ongoing risk of HPV infection due to recurrence of previously acquired and controlled infections as well as risks of new acquisitions," concluded the researchers. Reference Rositch AF, Patel EU, Petersen MR, Quinn TC, Gravitt PE, Tobian AAR. Importance of lifetime sexual history on the prevalence of genital human papillomavirus among unvaccinated adults in NHANES: implications for adult HPV vaccination [published online July 25, 2020]. Clin Infect Dis. doi:10.1093/cid/ciaa1050 |
| Ask the Doctors: Boys, girls can benefit from HPV vaccine - Santa Maria Times Posted: 20 Aug 2020 10:40 AM PDT  Dear Doctor: Everyone talks about girls getting the HPV vaccine. But what about boys? Isn't it just as important for boys to be vaccinated as well? Dear Reader: You're referring to the vaccination for human papillomavirus, or HPV. And you're correct that the vaccination is important for both girls and boys. HPV is the most common sexually transmitted infection in the United States, and it can lead to several types of cancer later in life. About 80 million people in the U.S. are currently infected with some type of the virus. About 14 million more, mostly teens and young adults, become infected every year. HPV refers to a group of more than 200 related viruses. Of these, more than 40 are spread through direct sexual contact. The majority of HPV infections clear up on their own, often in about two years. The rest, however, can linger. They can lead to health problems that range from mild to life-threatening. Some cause genital warts and are considered to be low-risk. Others can cause cancers in different parts of the body. In women, certain types of HPV can cause cancer of the cervix, vulva and vagina. In fact, most cases of cervical cancer are associated with HPV. In men, the viruses can cause penile cancer. They can also lead to anal cancer, and to cancers of the mouth and throat, each of which can occur in either gender. Men can also be carriers of the types of HPV that put women at risk. The first HPV vaccine won approval from the Food and Drug Administration in 2006. Today, an updated vaccine protects against nine strains of HPV. It has been extensively tested and found to be safe. Side effects can include swelling, pain or bruising at the injection site. Some people report temporary headache, dizziness, fever or nausea. There is no evidence that the vaccine causes any long-term side effects. When administered before an individual becomes sexually active, the vaccine has been found to be highly effective in preventing the infections it targets. The HPV vaccine is recommended for all children and adults from ages 9 through 26. For anyone on the fence, consider this: HPV infections cause an estimated 35,000 cases of cancer in men and women each year. But since the advent of the vaccine, infections in teen girls that lead to genital warts and most HPV cancers have dropped 86%. Young adult women have seen a decline of 71%. And among vaccinated women, HPV-related precancers linked to cervical cancer have dropped 40%. As the data show, the HPV vaccine saves lives. Sign up now to get the most recent coronavirus headlines and other important local and national news sent to your email inbox daily. |
| You are subscribed to email updates from "hpv in women" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |


Comments
Post a Comment